CBT In The Water Supply
July 16, 2015
Epistemic status: Very speculative, <50% confidence, thinking out loud. Don’t let this turn you off therapy.
Here’s a vignette from cognitive-behavioral therapy book When Panic Attacks, heavily edited for length:
A chronically anxious medical school professor named Nate suffered from low-self-esteem and feelings of inadequacy. One day, Nate brought me a copy of his CV. I was blown away. He’d listed over sixty pages of research publications, prestigious awards, and keynote addresses he’d given at major conferences around the world. I asked Nate how he reconciled his low self-esteem with all of his accomplishments. He said that every time he looked at his CV, he felt discouraged and told himself that his colleagues’ research studies were far more rigorous and important than his own. He said his paper seemed “soft” and consisted primarily of theoretical work, rather than hard-core laboratory research with real tissue. He said “Dr. Burns, no matter how much I accomplish, it never seems good enough.”
Perfectionism was clearly one of Nate’s self-defeating beliefs. I suggested that Nate use the Pleasure/Perfection Balance Worksheet to test this belief. I told him to write “If I can’t do something perfectly, it’s not worth doing at all” on the top of the sheet, and asked him to list several activities in the left-hand column. I told him to predict how satisfying and rewarding each activity would be, to record how satisfying and rewarding it was afterwards, and to rate how perfectly he did each activity. That way he could find out of it was true that he only enjoyed the things he did perfectly.
The next week, Nate had some interesting results to share with me. One of his activities was giving the welcoming lecture ot the incoming class of medical students. Nate gave this lecture every year because he was considered to be the most charismatic speaker at the medical school. Nate predicted this lecture would be 70% satisfying, but his actual satisfaction as only 20%. This was surprising, since he’d received a thirty-second standing obation, and he’d rated his perfection level for the talk at 90%.
I asked Nate why his satisfaction rating was so low. He explained that he always got standing ovations, so he routinely timed them. The previous year, the medical students had stood and cheered for more than a minute at the end of his talk. This year, the only stood and cheered for half a minute. Nate felt disappointed and started worrying that he was over the hill.
The second entry on Nate’s Pleasure/Perfection Balance Worksheet was that [he fixed a broken pipe in his bathroom]. He had to make several trips to the hardware story to buy tools and parts and to get tips on how to do it, so he didn’t get the pipe fixed until 10 PM. How explained that any plumber could have fixed the pipe in five minutes, so he rated his perfection as 5%. But his satisfaction level for this activity was 100%. In fact, he felt exhilarated. Nate said it was the most satisfying thing he’d done in years.
The result of Nate’s experiment was not consistent with his belief that things weren’t worth doing unless he did them perfectly. It dawned on him that there were many sources of satisfaction in his life that he’d overlooked, such as taking a walk through the woods with his wife, even though neither of them were world-class hikers, playing squash with his son, even though neither of them were champions, or just going out with his family for ice cream cones on a warm summer evening.
This experiment had a significant impact on Nate’s feelings of self-esteem and on his career. He told me that his feelings of anxiety and inferiority decreased, and his productivity actually increased because he was no longer so worried about having to do everything so perfectly.
At first I assumed this story was made up, but the book claims these are based on real patients, and even mentions how the writer showed videos of some of these therapy sessions to his classes. Interesting. How about another?
Several years ago, I did a three-day intensive workshop for a small group of psychotherapists in Florida. A marriage and family therapist named Walter explained that he’d been struggling with anxiety and depression for several months because Paul, the man he’d lived with for eight years, had found a new lover and left him. He put his hand on his chest and said: “It feels real heavy, right here. There’s just a sense of loneliness and emptiness about the whole experience. It feels so universal and final. I feel like this pain is going to go on forever, until the end of time.”
I asked Walter how he was thinking and feeling about the breakup with Paul. What was he telling himself? He saidL “I feel incredibly guilty and ashamed, and it seems like it must have been my fault. Maybe I wasn’t skillful enough, attractive enough, or dynamic enough. Maybe I wasn’t there for him emotionally. I feel like I must have screwed up. Sometimes I feel like a total fraud. Here I am, a marriage and family therapist, and my own relationship didn’t even work out. I feel like a loser. A really, really big loser.”
Walter recorded these five negative thoughts on his daily mood log:
- I’ll never be in a loving relationship again
- I must be impossible to live with and impossible to be in a relationship with
- There must be something wrong with me
- I totally screwed up and flushed my life down the toilet
- I’ll end up as an old, fat, gray-haired, lonely gay man
He believed all of these thoughts very strongly.
You can see that most of Walter’s suffering results from the illogical way he’s thinking about the rejection. You could even say that Walter is treating himself far more harshly than Paul did. I thought the Double Standard Technique might help because Walter seemed to be a warm and compassionate individual. I asked wehat he’d say to a dear friend who’d been rejected by someone he’d been living with for eight years. I said “Would you tell him that there’s something wrong with him, that he screwed up his life and flushed it down the toilet for good?”
Walter looked shocked and said he’d never say something like that to a friend. I suggested we try a role-playing exercise so that he could tell me what he would say to a friend who was in the same predicament […]
Therapist (role-playing patient’s friend): Walter, there’s another angle I haven’t told you about. What you don’t understand is that I’m impossible to live with and be in a relationship with. That’s the real reason I feel so bad, and that’s why I’ll be alone for the rest of my life.
Patient (role-playing as if therapist is his friend who just had a bad breakup): Gosh, I’m surprised to hear you say that, because I’ve known you for a long time and never felt that way about you. In fact, you’ve always been warm and open, and a loyal friend. How in the world did you come to the conclusion that you were impossible to be in a relationship with?
Therapist (continuing role-play): Well, my relationship with [my boyfriend] fell apart. Doesn’t that prove I’m impossible to be in a relationship with?
Patient (continuing role-play): In all honesty, what your’e saying doesn’t make a lot of sense. In the first place, your boyfriend was also involved in the relationship. It takes two to tango. And in the second place, you were involved in a reasonably successful relationship with him for eight years. So how can you claim that you’re impossible to live with?
Therapist (continuing role-play:) Let me make sure I’ve got this right. You’re saying that I was in a reasonably successful relationship for eight years, so it doesn’t make much sense to say that I’m impossible to live with or impossible to be in a relationship with?
Patient (continuing-role-play:) You’ve got it. Crystal clear.
At that point, Walter’s face lit up, as if a lightbulb had suddenly turned on in his brain, and we both started laughing. His negative thoughts suddenly seemed absurd to him, and there was an immediate shift in his mood… after Walter put the lie to his negative thoughts, I asked him to rate how he was feeling again. His feeling of sadness fell all the way fromj 80% to 20%. His felings of guilt, shame, and anxiety fell all the way to 10%, and his feelings of hopelessness dropped to 5%. The feelings of loneliness, embarassment, frustration, and anger disappeared completely.
The book is quite long, and it’s full of stories like this. The author, who’s one of the top cognitive-behavioral psychiatrists in the world, describes his experience with the therapy as:
[When I first learned about this therapy, I thought] depression and anxiety seemed far too serious and severe for such a simplistic approach. But when I tried these methods with some of my more difficult patients, my perceptions changed. Patients who’d felt hopeless, worthless, and desperate began to recover. At first, it was hard to believe that the techniques were working, but I could not deny the fact that when my patients learned to put the lie to their negative thoughts, they began to improve. Sometimes they recovered right before my eyes during sessions. Patients who’d felt demoralized and hopeless for years suddenly turned the corner on their problems. I can still recall an elderly French woman who’d been bitterly depressed for more than fifty years, with three nearly-successful suicide attempts, who started shouting “Joie de vivre! Joie de vivre!” (“joy of living”) one day in my office. These experiences made such a strong impact on me that I decided my calling was in clinical work rather than brain research. After considerable soul-searching, I decided to give up my research career and become a full-time clinician. Over the years, I’ve had more than 35,000 psychotherapy sessions with depressed and anxious patients, and I’m every bit as enthusiastic about CBT as when I first began learning about it.
Okay. I am not one of the top cognitive-behavioral therapists in the world. I’ve been studying formal cognitive-behavioral therapy for about a week now, and been doing untrained ad hoc therapy on inpatients for a couple years. But I’ve also gotten to observe a lot of other people doing therapy, and talked to people who have had therapy, and treated patients who were simultaneously undergoing therapy, and the impression I got was very different.
Dr. Burns asks patients to question whether their anxiety and their negative thoughts are rational, and their faces light up and all of their psychiatric problems suddenly melt away.
The therapists I’ve seen ask patients to question whether their anxiety and their negative thoughts are rational, ever so tactfully, and the patients say “No shit, Sherlock, of course they aren’t, but just knowing that doesn’t help or make them go away, and I’ve been through this same spiel with like thirty people already. Now shut up and give me my Xanax.”
In my last post, someone asked what to do if they found cognitive-behavioral therapy hokey and patronizing. I said, only half joking, that “if you don’t like hokey patronizing things, CBT may not be for you.” I know it’s mean, and pessimistic, but everyone I’ve talked to has had pretty much the same experience. I used to attribute this to my friends being pretty smart, and maybe CBT was aimed as less intelligent people, but Nate The Genius Medical School Professor seems pretty smart. So does Walter The Therapist. Burns’ book includes a bunch of other vignettes about high-powered lawyers, graduate students, et cetera. They all find his suggestions of “Well, have you considered that your irrational negative thoughts might not be rational?” super life-changing.
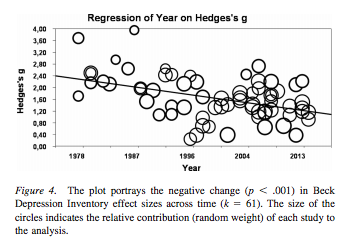
You might have read the study this graph comes from: The Effects of Cognitive-Behavioral Therapy As An Anti-Depressive Treatment Is Falling: A Meta-Analysis. As you can see, the Hedges’ g declined from about 2.5 in 1980 to around 1 today. The latest embarrassing set of results now show CBT doing no better than its old nemesis psychoanalysis. Why?
There are a lot of possible explanations. The smart money is always on “it never worked very well, but we’re finally doing studies that aren’t hopelessly biased”, but the analysis doesn’t find a clear difference in study quality. Other suggestions are that therapists have gotten less committed over time, or that the patient populations has changed. All of these sound reasonable. But let me mention one more possibility.
Every so often, psychiatrists joke about how so many people are depressed we might as well put Prozac in the water supply. Sometimes we say the same thing about lithium, although in that case we’re not joking.
Nobody’s ever talked about putting cognitive-behavioral therapy in the water supply, but insofar as that’s meaningful at all I would say we’ve kind of done it. Cognitive-behavioral ideas, like perfectionism, excessive self-blame, conditional versus unconditional self-respect, deep breathing, goal-setting, et cetera have become basic parts of popular culture. The whole self-esteem movement isn’t exactly cognitive-behavioral, but it’s certainly allied, and it certainly represents a shift to a style of thinking about the self and about psychology in a way that’s much more fertile for cognitive-behavioral ideas. Inside Out was kind of “Cognitive Behavioral Therapy: The Movie”.
Although the particular book I’m reading is from 2006, Burns himself was one of Aaron Beck’s original students and one of the first cognitive-behavioral therapists ever. I wonder how many of these patients who seem absolutely shocked to realize that maybe their anxiety isn’t rational come from that very early period.
It’s very hard to track changes in people’s basic beliefs about psychology. I was flabbergasted to learn that until Dr. Benjamin Spock’s landmark 1940s book on child care, parents were told not to hug, kiss, or show affection to babies, because that would coddle them and make them weak, pampered adults. Before that, parents interacted with their kids much less, and it was assumed that siblings and nannies and friends would raise them, or they would raise themselves. It’s easy to read books about ancient Greece and not notice that they have a completely different view of the role of the self/individual than we do. So it wouldn’t surprise me if a lot of the psychology we consider “obvious” is CBT that has seeped out into the water supply over the past thirty years.
If that were true, it would explain why CBT is no longer as effective – it’s just telling people things they already know.
It could be fairly asked: then why isn’t everybody already better? Depression seems to be increasing, though there’s a lot of argument about exactly how much; that doesn’t sound like what would happen if everyone were automatically getting a background level of therapy.
Here’s a theory, though it’s on even shakier ground than the other one. The meta-analysis proposes that CBT may have lost some placebo effect over time because patients no longer think of it as The Exciting New Thing. I’m not sure I can go along with that – my own analysis of psychotropic medications suggests patients very much prefer the old ones for some reason. But a big part of psychotherapy is placebo effect, so they might be on to something.
What part of psychotherapy provides the placebo? Is it going to the clinic? Talking to the therapist? Hearing fancy words like “self-estimation”? Doing worksheets?
One thing a lot of therapies have in common is that they provide the feeling of insights. For example, psychoanalysts are very good at coming up with surprising-but-plausible ways that your current problems are linked to things that happened to you as a child; the usual result is a patient feeling enlightened, like “You’re right, the leg pain that’s been bothering me is in the same part of my leg that accidentally brushed up against my mother’s breast one time when I was seven, that’s pretty interesting.”
Suppose that in the old days, CBT was an insight a minute and you were constantly hearing surprising things you’d never thought about before. And nowadays, you’re kind of absorbing a lot of those things by osmosis without it seeming too insightful, and then the therapy itself is anticlimactic. Could that lessen the placebo effect enough to account for the data?
I don’t know. Maybe after I’ve been training in formal CBT for more than a week, I’ll have more data and can report back to you.
EDIT: Sarah writes: “In a way, seeing CBT stuff in pop culture inoculates people, I think. People will get as far as noticing “this negative thought is an anxiety symptom”, but not as far as *actually reversing it*. When people hadn’t heard of CBT, they first got the “this negative thought is irrational” message in a context when they were actively working on their problems, so they followed through with the ‘hard’ step of actually reversing the thought. Now, people run into the revelation that the ‘inner critic’ is wrong just by browsing facebook, when they’re *not* actively trying to fight their anxiety problems, so the revelation loses its force.”
EDIT 2: Paul Crowley points out a very similar theory in The Guardian